Ehlers-Danlos Syndrome: A Patient and Provider Perspective
Hello and Welcome to my blog!
I first heard about hypermobility disorders such as Marfan’s and Ehlers-Danlos (EDS) in graduate school. We were taught that these patients were too dangerous to touch, work on, or adjust and that we should avoid treating them and refer them to pain management. I had no reason to question this, until I was finally diagnosed with hEDS by a chiropractor with a neurologic diplomat. I had been responding poorly to traditional chiropractic care for a while now, and being in chiropractic school, this was making me second guess my own career. If I couldn’t get better with chiropractic care, how was I going to help patients with techniques that didn’t help me? How could I believe in the power of the adjustment when I couldn’t heal with that same power?
How hEDS Affected Dr. Super
As a chiropractic graduate student, I had no experience receiving chiropractic care until I enrolled at Palmer College of Chiropractic in Davenport, Iowa. I remember walking through the club fair that first week and seeing so many different chiropractic techniques. I truly thought all chiropractors did the same “snap, crackle, pop” adjustments. I was shocked to learn there were over 200 chiropractic techniques, each viewing treatment through a unique lens.
There was Activator Club, Adjusting Ninjas, Gonstead Club, Motion Palpation Club, NUCCA Club, SOT Club, Pediatric Club, Animal Chiropractic Club, and at least 30 more I had never heard of. An upperclassman from a long line of chiropractors told me to “steer clear of the weirdos” and avoid clubs that didn’t do aggressive manual adjustments because “that gentle stuff doesn’t work” and “how can they believe they can adjust with light touch?” I didn’t know any better, so I avoided the clubs with reputations for “strangeness” or “imaginary care” that used gentle or low-force techniques.
It wasn’t until I started going to the student clinic for my first course of chiropractic care that I began questioning what “effective” techniques actually were. I had been having migraines several times a week for years, and I felt like I was always in pain everywhere. I was excited to start feeling better with Gonstead technique, but the adjustments left me in more pain afterward. My student intern joked that I was a “confidence killer” because he couldn’t properly isolate adjustments in my neck or back. His staff doctor told me that petite women are the hardest to adjust because they’re usually so “bendy” that it’s difficult to lock out the joint for a good adjustment. He suggested using more force and adding more bend to match my flexibility. As you can imagine, this was even more uncomfortable, and I felt like they were trying to crush me instead of cure me.
I was eventually referred to a Diversified staff doctor, as people usually respond better to that technique. But it ended up being the same song and dance. Then they sent me to Cox Flexion-Distraction, which really aggravated my low back, so they tried Thompson technique. This worked well for a while, but the pain was stubborn, and I had to be seen every week or all my symptoms would return. They said the last stop for me was the Activator doctor—a technique many students laughed at. It did help, but I still couldn’t hold my adjustments, and I was still having migraines several times a month. I would leave the clinic, look both ways to cross the street, feel my neck “pop” out of alignment again, and immediately the headache would return.
It turned out Activator wasn’t my last stop. My staff doctor recommended NUCCA care. This technique was highly specialized and required a referral. I was not thrilled—I had heard NUCCA was the most mocked technique on campus. How could a gentle touch, once a month, on a single bone fix all my issues?
Well… it worked pretty darn well. The first few adjustments made me feel worse for a couple of days, but by my second and third visit, I was feeling better and holding my adjustments longer. After six adjustments over six months, my migraines were completely gone. That felt like a miracle.
I asked my staff doctor why this technique worked so well for me when nothing else did. He told me it was because I was hypermobile and most likely had EDS. I was confused because I’d been taught to think of EDS patients as those with clubfoot, osteogenesis imperfecta, or obvious mobility disorders. But when he reviewed my history and symptoms, everything strongly indicated hEDS. Suddenly everything “clicked,” and for the first time I understood why my body struggled so much.
Besides being extraordinarily flexible, there were so many indicators. As a kid, I was immune to lidocaine and novocaine, and I could still feel everything during dental procedures. I woke up during shoulder surgery at age 23 because I metabolize anesthetics too quickly. Muscle relaxers and pain meds aren’t effective for my spasms or joint pain. I constantly dislocated my shoulders and kneecaps and sprained my ankles while running, all without any major injury. I healed quickly on the surface, but always had thin, wrinkly, white scars, and the internal scarring after surgery was a nightmare to recover from. My pain often migrated from place to place as my body tried to stabilize itself, especially after injuries.
I liked sitting or sleeping with my legs twisted around each other because it made me feel more stable. I have astigmatism. I was diagnosed with dysautonomia, POTS, slipping rib syndrome, fibromyalgia, leaky gut, and gastroparesis. I had heavy, irregular periods; varicose veins since elementary school; cellulite no matter how small or toned I was; and stretch marks before puberty and without weight gain. My skin is almost see-through, with blue veins branching visibly across my body. I have bilateral piezogenic papules, TMJ issues, constantly cold hands and feet, heart arrhythmia, poor proprioception, easy bruising, and a long list of other subtle signs of hEDS—with possible vascular involvement as well.
Now that I finally knew what I had, I had to figure out what to do about it. I learned that my body needed a completely different approach for almost everything. My physical therapy changed. My chiropractic care changed. My massage techniques changed. My diet changed. My sleeping posture changed. How I worked out changed. And most importantly, how I interpreted my symptoms changed.
And that transformed how I treat my patients—especially those with chronic pain related to hEDS.
So for those who don’t have this condition… what exactly is hEDS?
How hEDS Affects a Patient
Hypermobile Ehlers–Danlos syndrome is a heritable connective tissue disorder primarily characterized by joint hypermobility, chronic pain, and soft tissue fragility. Since connective tissue is present throughout the entire body, symptoms are multi-systemic and they don’t just affect the joints.
Common symptoms of hEDS include joint instability and frequent subluxations or dislocations (even with normal movements like rolling over in bed), chronic musculoskeletal pain (often diffuse and disproportionate to an observable injury), soft, elastic, or velvety skin that may bruise easily or scar poorly. These patient are also often diagnosed with Autonomic Dysfunction (including POTS-like symptoms such as dizziness, heart palpitations, or heat intolerance), gastrointestinal issues (including bloating, constipation, reflux, or motility problems), fatigue and sleep disturbances, proprioceptive dysfunction leading to clumsiness or frequent minor injuries (bumping into doorframes, walls, or desks), anxiety or mood symptoms, sometimes related to dysautonomia or chronic pain, and a plethora of other symptoms.
Why Symptoms Differ from Person to Person
The variability in expression of hEDS is enormous. We are still researching and trying to understand the genetic abnormalities of people with hEDS, and the disorder is on a spectrum; this means one person with the same condition can have a completely different set of symptoms than someone else with the same condition. Even among family members with the same condition, one person may experience disabling pain and frequent dislocations, while another has only mild hypermobility or fatigue. Research has also shown a difference in symptom severity based on hormones such as estradiol and testosterone. Someone who went through a puberty with more testosterone would have a decrease in symptom severity, while someone who had a puberty with more estradiol would have an increase in symptoms. This can also explain why individuals may have a change of symptom severity that correlates with hormone fluctuations during their menstrual cycle or why a FTM (female to male) transitioning individual may have a decrease of symptom severity while taking testosterone.
This variation likely also stems from:
Genetic heterogeneity: the exact genetic basis of hEDS remains unknown, unlike other EDS types with clearly defined mutations for things such as osteogenesis imperfecta.
Environmental and lifestyle factors: Injury history, physical activity, hormonal changes, and stress can modulate symptom severity.
Comorbidities: Many patients develop overlapping conditions like fibromyalgia, mast cell activation syndrome, or dysautonomia, which can amplify or complicate symptoms.
Differences in nervous system sensitization: Chronic pain and proprioceptive dysfunction can alter how the brain interprets body signals, leading to wide-ranging symptom perception. Individuals can also vary greatly in their tolerance of pain based on how long or how many symptoms they are exposed to.
The Difficulty of Getting Diagnosed
Getting an accurate hEDS diagnosis is notoriously difficult. Since the entire family of conditions—including hEDS and HSD—is perceived as rare, healthcare professionals, care organizations, and policymakers may assume these disorders are not relevant to their work. As a result, priority tends to be given to more common conditions that affect larger populations. I have unfortunately referred several patients to providers to discuss how hEDS is affecting their condition or care, and the provider responds with “that doesn’t matter or change anything”. Several other factors that contribute to the difficulty of getting diagnosed include
Lack of definitive testing: There is currently no conclusive genetic test for hEDS, so diagnosis relies on clinical criteria (Beighton score, systemic features, and exclusion of other EDS types). Studies have shown that about 90% of people with hEDS will show a negative genetic test, even though they have the condition!
Overlapping symptoms: hEDS mimics or coexists with many other conditions — chronic fatigue, fibromyalgia, anxiety, IBS — which can mislead clinicians. This also results in patients seeing many different healthcare professionals without getting helpful or accurate answers to their healthcare concerns.
Limited clinician training: Many medical professionals receive minimal education on connective tissue disorders, leading to underrecognition. This also results in clinicians dismissing patients and writing their symptoms off as “not significant”.
Gender bias: Because hEDS is more frequently diagnosed in women, symptoms are sometimes misattributed to psychological causes (“stress,” “somatization,” “anxiety”). Many women experience discrimination in healthcare and are told to “toughen up”. It is also more difficult to diagnose an adult male as their symptoms may be reduced due to the amount of testosterone.
As a result, patients often spend years or even decades seeking answers, seeing numerous specialists before receiving a diagnosis — a phenomenon sometimes called the “diagnostic odyssey.” My goal as a healthcare provider is to connect the dots and accurately diagnose patients, so that they can finally get the answers, and care they deserve.
Discrimination and Dismissal in Healthcare
Unfortunately, many hEDS patients experience medical gaslighting (for more about this, read my blog post “You’re Not Crazy: a Look at Medical Gaslighting” https://www.drsupershouseofhealth.com/blog/youre-not-crazy-a-look-at-medical-gaslighting). In these instances, a patients symptoms are minimized, doubted, or dismissed. Some of my patients have even been called “frequent flyers” or “attention seeking”, which is highly offensive. This also results in patients refusing to get care when they need it the most out of fear that they will be dismissed or invalidated.
Common experiences also include:
Being told they are “just flexible” or that their pain is exaggerated. I was told by one provider that I “can’t be afraid of moving and you have to stop sitting on your couch eating bon-bons all day”. Anyone who knows me can see how absolutely ridiculous that statement was!
Providers labeling them as “drug-seeking” or “attention-seeking” due to chronic pain complaints. These patients often don’t respond to common muscle relaxers or pain medications, and they don’t want to be on medication the rest of their life. Some providers interpret this as the patient’s attempt to be prescribed “harder stuff”.
Repeatedly being referred to psychological or psychiatric care instead of being medically evaluated. In my opinion, therapy should be utilized by everyone, but only obtaining this type of treatment fails to address the real issues affecting the patient.
Having legitimate injuries or dislocations questioned because imaging sometimes fails to show clear pathology. With my own right shoulder MRI, it showed everything was “within normal limits”, but when my surgeon finally gave me an “exploratory scoping surgery for my peace of mind” he said it was the worst shoulder injury he has treated in 35 years!
This systemic bias creates profound emotional and physical harm. It erodes trust in the medical system and often forces patients to become their own advocates, sometimes researching and educating their providers about their condition. I often refer patients to https://www.ehlers-danlos.com/ which has resources on it for patients and providers to learn more about hEDS and other EDS conditions. It includes helpful diagnostic criteria, providers lists, and surgical considerations for providers to learn how to modify their approach to safely treat EDS patients.
Diagnosing hEDS in the Office
Since hEDS is a complex, multi-systemic connective tissue disorder that can range from mildly symptomatic to profoundly disabling, and no two patients experience it the same way, and because the condition remains poorly understood and underdiagnosed, many endure years of disbelief and inadequate care. The combination of diagnostic uncertainty, symptom invisibility, and systemic bias contributes to discrimination and invalidation within healthcare — an issue that continues to call for education, empathy, and reform. It is my deepest honor to be able to help patients connect the dots and help then learn that their experiences are valid and real.
The first thing that clues me in to a possible hEDS diagnosis is when someone says “everything is broken and no one can find anything wrong”. This patient may have been to every specialist under the son. Rheumatology, cardiology, neurology, OGBYN, an orthopedic specialist, etc.Each clinician will have their own idea of what is wrong, and the patient is either misdiagnosed and does not respond to treatment, or they receive no diagnosis at all. I may also notice upon evaluation that they have a pattern of joint hypermobility with joint pain accompanied by muscle hypertonicity (too tight). A detailed patient history may also reveal clues such as hip dysplasia as a baby, easy bruising, multiple or recurring hernias, chronic and widespread pain that moves around the body, painful and irregular periods, chronic fatigue, poor sleep, GI issues, mast cell or histamine response issues, poor heat tolerance, anxiety, headaches, or migraines. It is at this point that I take out my hEDS diagnostic criteria worksheet and evaluate for an hEDS diagnosis.
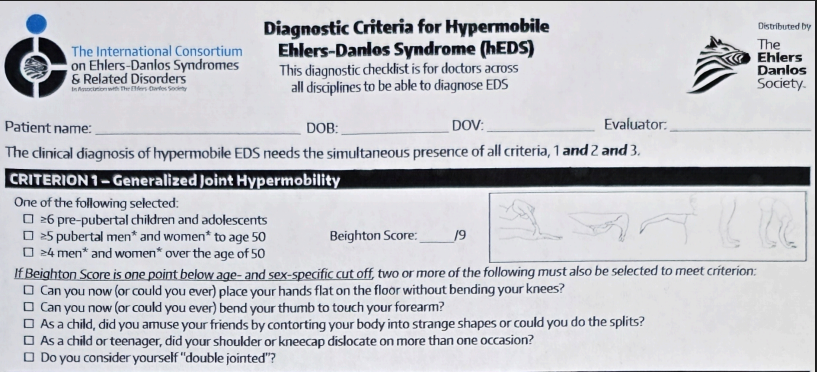
Imagine 1: The initial evaluation explores the hypermobility component and measured angles of common hypermobile joints in the body including the hands, elbows, knees, and back.
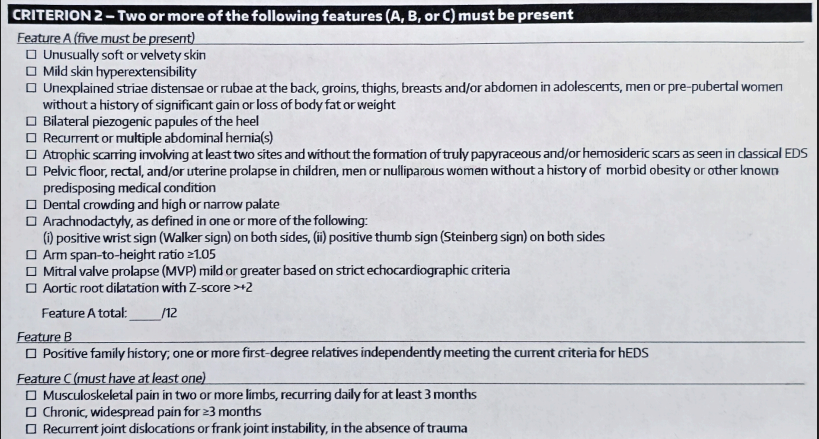
Image 2: Goes over other insidious symptoms which may help support an hEDS diagnosis. This may also clue the provider in on whether the patient may have a vascular component as well.
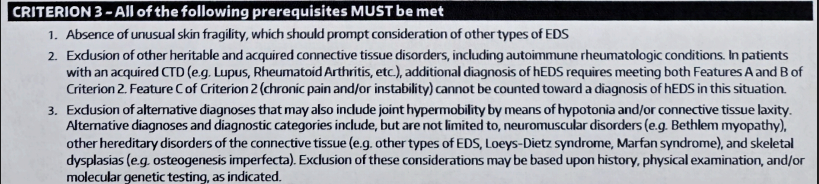
Image 3: Exclusion criteria to help rule in or out other conditions that can mimic hEDS symptoms. This can be complicated by patients that have multiple co-morbidities.
Once I have an hEDS diagnosis for a patient, I am able to pick techniques and procedures that are safe and effective at relieving their discomfort, increases their proprioception, and help their nervous system better regulate and become less sensitive to stimuli. Many of my patients with hEDS report decreased pain frequency and severity, decreased headache, better mood and hormone regulation, and decreased autoimmune or MCAS (mast cell activation syndrome) symptoms. As a chiropractor, I understand how the nervous system is affected by this instability and how gentle and effective chiropractic care can help aid the body in managing this condition. As a patient and a clinician, I have learned so much about hEDS from my own patients and I consider them to be my greatest resource. Many of them have shared their journey with me, which includes their investigation and research into how hEDS has affected their body, and what they have found helps the most.
Genetic testing can help find what supplements will be support a patient with hEDS, as many are not able to properly methylate various forms of vitamins. Myofascial release of Craniosacral therapy techniques can be an effective and gentle way to help “unwind” the various injury patterns most hEDS patients face. Doing gentle stabilization exercises to increase postural strength and stability can be more effective than stretching and aggressive PT protocols when relieving muscle spasms. KT tape can also be helpful when supporting joint injuries while in recovery. Daily Vitamin C can help support a healthy and regular menstrual cycle as the irregular or heavy bleeding can be related to a collagen clotting factor disorder. Many other examples exist where my patients have become the biggest supporting advocates for other hEDS patients (including myself). At our office, patients and providers are here to help discover and share coping strategies, information about providers who are familiar with the condition, and personal experiences to help validate the reality that is hEDS. I know this blog post is a lot of information, but it is still only scratching the surface of what life looks lie for an hEDS patient. I wanted to leave you with a quote from our very own Hailee (front desk) who was one of my first hEDS patients at 15:
“Living with hEDS means my joints rarely stay where they’re supposed to, and every day feels unpredictable. I can go from feeling okay to struggling to move without pain, and some mornings I wake up aching from nothing more than sleeping. My muscles are constantly working overtime to stabilize my loose joints, leaving them tight, tired, and worn out.
Chiropractic care has given me a kind of freedom I didn’t think was possible. I’ve learned how to walk in a way that supports my body and keeps my hips from grinding. When my back locks up or my knees ache from hyperextension, an adjustment can make me feel like a new person. Even the strengthening exercises I was given have become a morning routine I actually look forward to.
Having a chiropractor who understands hEDS has helped my body feel more like the 23-year-old it’s supposed to be. Since starting care, I don’t hurt every day—and that change has made a huge impact on my life.”
I hope this post reaches someone who truly needs this information. Whether you’re learning about yourself or seeking answers for a loved one, I hope these resources bring clarity, insight, and encouragement. There is hope for people living with chronic pain and multiple co-morbidities—yes, even for those with hEDS.
Every day, I’m honored by the trust my hEDS patients place in my care, including my own infant daughter. As a mother, I’m deeply grateful to have the knowledge and tools to support her as she grows with this often misunderstood condition. My goal is to help ensure that hEDS never keeps her from living a long, fulfilling, and healthy life.
If you or someone you love is navigating this journey, please remember that you are not alone—and you are not without options. With the right support, understanding, and guidance, life with hEDS can be managed with far more hope and strength than many people are led to believe. My goal in sharing this is to empower you to seek answers, advocate for yourself, and know that better days are possible.
Thank you for taking the time to read, learn, and grow with me. For more information:
https://www.ehlers-danlos.com/what-is-eds/
ADIO,
Dr. Super